AREA TEMATICA: Ibd
Authors:
Susanna Faenza1, Marco Valvano1,2, Fabio Cortellini3, Antonio Vinci4,5, Fabio Ingravalle5, Mauro Calabrò1, Lorenza Scurti1, Mariagiulia Di Nezza1, Sergio Valerio6, Angelo Viscido1, Giovanni Latella1
Affiliations:
- Gastroenterology, Hepatology and Nutrition Division, Department of Life, Health and Environmental Sciences, University of L’Aquila, Italy
- Division of Gastroenterology, Galliera Hospital, Genoa, Italy
- Gastroenterology and Digestive Endoscopy, AUSL Romagna, Rimini, Italy
- Azienda Regionale Emergenza Sanitaria ARES 118, Rome, Italy
- Doctoral School of Nursing Sciences and Public Health, University of Rome “Tor Vergata,” Rome, Italy
- Alimenta – Nutrition and Wellness Studio, Foggia, Italy
Background and aims:
Inflammatory bowel diseases (IBD) are associated with malnutrition and micronutrient deficiencies, which may influence disease activity and outcomes. This study aimed to evaluate the relationship between nutritional status, micronutrient deficiencies, and clinical as well as biochemical disease activity in IBD patients.
Methods:
This cross-sectional study included adult patients with a confirmed diagnosis of IBD. Clinical and biochemical evaluations were performed, and micronutrient assessment comprised iron, ferritin, vitamin B12, vitamin D, and folate, together with hemoglobin and albumin. Disease activity was defined according to validated clinical scores and fecal calprotectin levels. Pearson correlation and ROC analyses were conducted to assess associations and discriminatory accuracy.
Results:
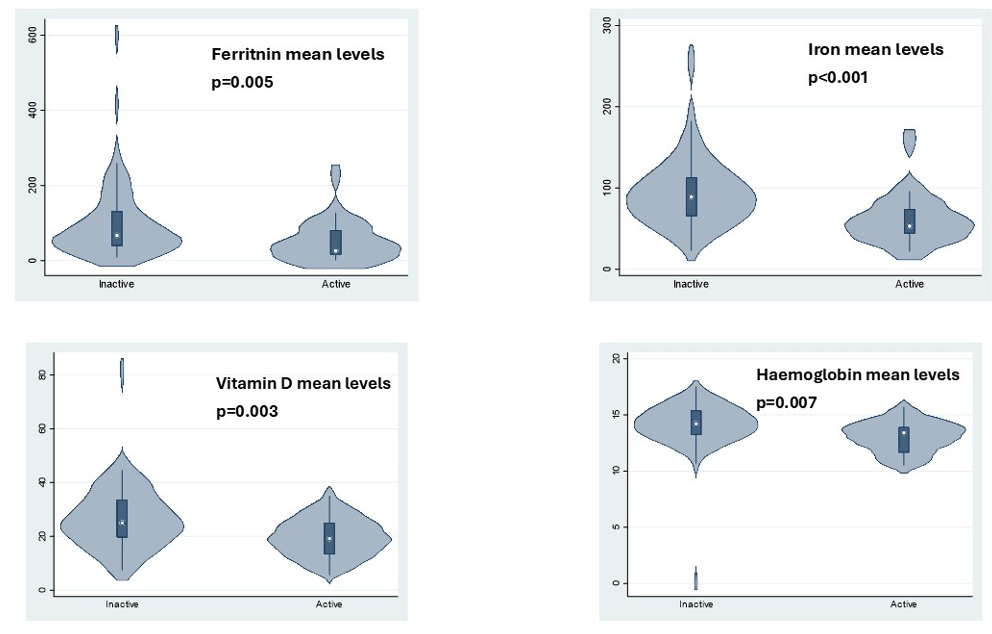
A total of 110 patients were enrolled (40 Crohn’s disease, 70 ulcerative colitis). Twenty-two percent showed clinical activity, and 34% had elevated calprotectin. Patients with active disease had significantly lower hemoglobin, iron, ferritin, and vitamin D levels compared to inactive patients (p = 0.007, p < 0.001, p = 0.005, and p = 0.003, respectively). No significant differences were observed for folate, vitamin B12, or albumin. ROC analyses showed that iron (AUC 0.76, p < 0.001) and vitamin D (AUC 0.68, p = 0.013) had the highest discriminatory power, though suboptimal. Multivariate analysis confirmed ferritin as independently associated with disease activity (OR 0.98; p = 0.015).
Conclusions:
Hemoglobin, iron, ferritin, and vitamin D correlate with disease activity in IBD, but their discriminatory accuracy remains limited. Folic acid, vitamin B12, and albumin do not appear reliable markers of activity. Larger prospective studies are warranted to better define the role of micronutrient assessment in disease monitoring.
Bibliography:
- Gkikas K, Gerasimidis K, Milling S, Ijaz UZ, Hansen R, Russell RK. Dietary Strategies for Maintenance of Clinical Remission in Inflammatory Bowel Diseases: Are We There Yet? Nutrients. 2020;12:2018.
- Pasternak G, Chrzanowski G, Aebisher D, Myśliwiec A, Dynarowicz K, Bartusik-Aebisher D, Sosna B, Cieślar G, Kawczyk-Krupka A, Filip R. Crohn’s Disease: Basic Characteristics of the Disease, Diagnostic Methods, the Role of Biomarkers, and Analysis of Metalloproteinases: A Review. Life. 2023;13:2062.
- Li L, Cheng R, Wu Y, Lin H, Gan H, Zhang H. Diagnosis and Management of Inflammatory Bowel Disease. J Evid Based Med. 2024;17:409–433.
- Wang R, Li Z, Liu S, Zhang D. Global, Regional and National Burden of Inflammatory Bowel Disease in 204 Countries and Territories from 1990 to 2019: A Systematic Analysis Based on the Global Burden of Disease Study 2019. BMJ Open. 2023;13:e065186.
- Aebisher D, Bartusik-Aebisher D, Przygórzewska A, Oleś P, Woźnicki P, Kawczyk-Krupka A. Key Interleukins in Inflammatory Bowel Disease—A Review of Recent Studies. Int J Mol Sci. 2024;26:121.
- Chang JT. Pathophysiology of Inflammatory Bowel Diseases. N Engl J Med. 2020;383:2652–2664.
- Kotla NG, Rochev Y. IBD Disease-Modifying Therapies: Insights from Emerging Therapeutics. Trends Mol Med. 2023;29:241–253.
- Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn’s Disease. Lancet. 2017;389:1741–1755.
- Flynn S, Eisenstein S. Inflammatory Bowel Disease Presentation and Diagnosis. Surg Clin N Am. 2019;99:1051–1062.
- Froehlich-Grobe K, Jones D, Businelle MS, Kendzor DE, Balasubramanian BA. Impact of Disability and Chronic Conditions on Health. Disabil Health J. 2016;9:600–608.
- Chimienti M, Morlino G, Ingravalle F, Vinci A, Colarusso E, De Santo C, Formosa V, Gentile L, Lorusso G, Mosconi C, et al. Unemployment Status Subsequent to Cancer Diagnosis and Therapies: A Systematic Review and Meta-Analysis. Cancers. 2023;15:1513.
- Bisgaard TH, Allin KH, Keefer L, Ananthakrishnan AN, Jess T. Depression and Anxiety in Inflammatory Bowel Disease: Epidemiology, Mechanisms and Treatment. Nat Rev Gastroenterol Hepatol. 2022;19:717–726.
- Yanai H, Feakins R, Allocca M, Burisch J, Ellul P, Iacucci M, Maaser C, Zilli A, Zidar N, Wilkens R, et al. ECCO-ESGAR-ESP-IBUS Guideline on Diagnostics and Monitoring of Patients with Inflammatory Bowel Disease: Part 2. J Crohns Colitis. 2025;19:jjaf106.
- De Bernardi A, Bezzio C, Puricelli M, Gilardi D, Saibeni S. Combining Advanced Targeted Therapy in Inflammatory Bowel Disease: Current Practice and Future Directions. J Clin Med. 2025;14:590.
- Plevris N, Lees CW. Disease Monitoring in Inflammatory Bowel Disease: Evolving Principles and Possibilities. Gastroenterology. 2022;162:1456–1475.e1.
- Colombel JF, D’haens G, Lee WJ, Petersson J, Panaccione R. Outcomes and Strategies to Support a Treat-to-Target Approach in Inflammatory Bowel Disease: A Systematic Review. J Crohns Colitis. 2020;14:254–266.
- Maaser C, Sturm A, Vavricka SR, Kucharzik T, Fiorino G, Annese V, Calabrese E, Baumgart DC, Bettenworth D, Borralho Nunes P, et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial Diagnosis, Monitoring of Known IBD, Detection of Complications. J Crohns Colitis. 2019;13:144–164.
- Weisshof R, Chermesh I. Micronutrient Deficiencies in Inflammatory Bowel Disease. Curr Opin Clin Nutr Metab Care. 2015;18:576–581.
- Svolos V, Gordon H, Lomer MCE, Aloi M, Bancil A, Day AS, Fitzpatrick JA, Gerasimidis K, Gkikas K, et al. ECCO Consensus on Dietary Management of Inflammatory Bowel Disease. J Crohns Colitis. 2025;jjaf122.
- Zhang Y, Zhang L, Gao X, Dai C, Huang Y, Wu Y, Zhou W, Cao Q, Jing X, Jiang H, et al. Impact of Malnutrition and Sarcopenia on Quality of Life in Patients with Inflammatory Bowel Disease: A Multicentre Study. J Cachexia Sarcopenia Muscle. 2023;14:2663–2675.
- Hashash JG, Elkins J, Lewis JD, Binion DG. AGA Clinical Practice Update on Diet and Nutritional Therapies in Patients with Inflammatory Bowel Disease: Expert Review. Gastroenterology. 2024;166:521–532.
- Del Pinto R, Pietropaoli D, Chandar AK, Ferri C, Cominelli F. Association Between Inflammatory Bowel Disease and Vitamin D Deficiency. Inflamm Bowel Dis. 2015;21:2708–2717.
- Valvano M, Magistroni M, Cesaro N, Carlino G, Monaco S, Fabiani S, Vinci A, Vernia F, Viscido A, Latella G. Effectiveness of Vitamin D Supplementation on Disease Course in Inflammatory Bowel Disease Patients: Systematic Review with Meta-Analysis. Inflamm Bowel Dis. 2024;30:281–291.
- Wallace C, Gordon M, Sinopoulou V, Limketkai BN. Vitamin D for the Treatment of Inflammatory Bowel Disease. Cochrane Database Syst Rev. 2023;2023:CD011806.
- Valvano M, Capannolo A, Cesaro N, Stefanelli G, Fabiani S, Frassino S, Monaco S, Magistroni M, Viscido A, Latella G. Nutrition, Nutritional Status, Micronutrients Deficiency, and Disease Course of Inflammatory Bowel Disease. Nutrients. 2023;15:3824.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet. 2007;370:1453–1457.
- Kucharzik T, Taylor S, Allocca M, Burisch J, Ellul P, Iacucci M, Maaser C, Baldin P, Bhatnagar G, Ben-Horin S, et al. ECCO-ESGAR-ESP-IBUS Guideline on Diagnostics and Monitoring of Patients with Inflammatory Bowel Disease: Part 1. J Crohns Colitis. 2025;19:jjaf107.
- Bischoff SC, Bager P, Escher J, Forbes A, Hébuterne X, Hvas CL, Joly F, Klek S, Krznaric Z, Ockenga J, et al. ESPEN Guideline on Clinical Nutrition in Inflammatory Bowel Disease. Clin Nutr. 2023;42:352–379.
- Gubatan J, Moss AC. Vitamin D in Inflammatory Bowel Disease. Curr Opin Gastroenterol. 2018;34:217–225.
- Massironi S, Viganò C, Palermo A, Pirola L, Mulinacci G, Allocca M, Peyrin-Biroulet L, Danese S. Inflammation and Malnutrition in Inflammatory Bowel Disease. Lancet Gastroenterol Hepatol. 2023;8:579–590.
- Cesaro N, Valvano M, Monaco S, Stefanelli G, Fabiani S, Vernia F, Necozione S, Viscido A, Latella G. The Role of New Inflammatory Indices in the Prediction of Endoscopic and Histological Activity in Inflammatory Bowel Disease Patients. Eur J Gastroenterol Hepatol. 2025;37:24–32.
- Ananthakrishnan AN, Khalili H, Higuchi LM, Bao Y, Korzenik JR, Giovannucci EL, Richter JM, Fuchs CS, Chan AT. Higher Predicted Vitamin D Status Is Associated with Reduced Risk of Crohn’s Disease. Gastroenterology. 2012;142:482–489.
- MacMaster MJ, Damianopoulou S, Thomson C, Talwar D, Stefanowicz F, Catchpole A, Gerasimidis K, Gaya DR. A Prospective Analysis of Micronutrient Status in Quiescent Inflammatory Bowel Disease. Clin Nutr. 2021;40:327–331.
- Valvano M, Magistroni M, Mancusi A, D’Ascenzo D, Longo S, Stefanelli G, Vernia F, Viscido A, Necozione S, Latella G. The Usefulness of Serum Vitamin D Levels in the Assessment of IBD Activity and Response to Biologics. Nutrients. 2021;13:323.
- Battistini C, Ballan R, Herkenhoff ME, Saad SMI, Sun J. Vitamin D Modulates Intestinal Microbiota in Inflammatory Bowel Diseases. Int J Mol Sci. 2020;22:362.
Table 3. Normal levels of micronutrients and relative Odds Ratio and Area Under the Curve in active group (both clinical and calprotectin activity)
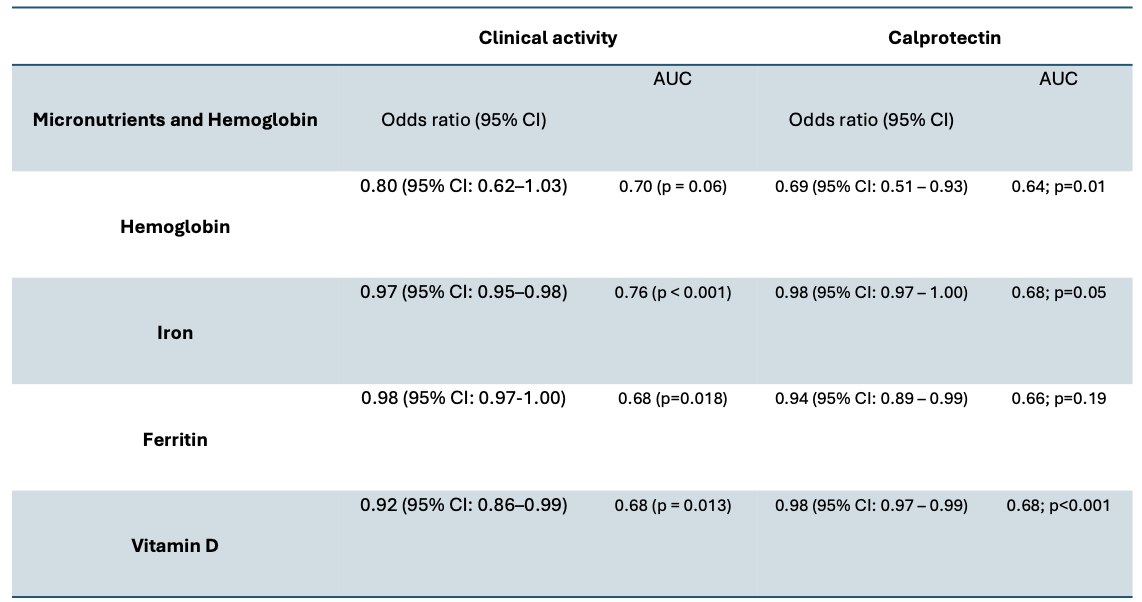
Figure 1. The boxplot shows the mean serum level of ferritin, iron, vitamin D and Hemoglobin among active and inactive groups.
VALUTA ABSTRACT
Vota ogni categoria
| Originality | |
| Clarity | |
| Rationale | |
| Objectives | |
| Endpoint measures | |
| Statistics | |
| Results | |
| Relevance | |
|
Media
|
|

|
|