AREA TEMATICA: Ibd
Authors:
Miriam Di Mattia1,2,*, Cesare Pane1,2, Valentina Petito3, Lamolinara A.1, Iezzi M.1, Elisa Foscarini3, Francesca Profeta3, Guia Becherucci3, Letizia Masi3, Sara Troisi1,2,3, Valeria Emoli3, Laura Turchini3, Antonio Gasbarrini3,4,5, Alfredo Papa4,5, Franco Scaldaferri3,4,5, Loris Riccardo Lopetuso1,2,4
Affiliations:
- Center for Advanced Studies and Technology (CAST), “G. d’Annunzio” University of Chieti-Pescara, Chieti, Italy
- Department of Medicine and Ageing Sciences, “G. d’Annunzio” University of Chieti-Pescara, Chieti, Italy
- CeMAD Translational Research Laboratories, Digestive Disease Center (CeMAD), Department of Medical and Surgical Sciences, Fondazione Policlinico Universitario “A. Gemelli” IRCCS, Rome, Italy
- IBD Unit, Digestive Disease Center (CeMAD), Department of Medical and Surgical Sciences, Fondazione Policlinico Universitario “A. Gemelli” IRCCS, Rome, Italy
- Department of Translational Medicine and Surgery, Catholic University of the Sacred Heart, Rome, Italy
Background and aims:
Short bowel syndrome (SBS) is a life-altering and life-threatening disease resulting from massive small bowel resections, often occurring in patients with Crohn’s disease (CD), a severe chronic gastrointestinal disorder characterized by the infiltration of inflammatory cells into the intestinal mucosa and submucosa1,2. Currently, no biomarkers indicate a higher risk of developing SBS or intestinal failure (IF); thus, the present study aims to evaluate the circulating cytokine/chemokine profile in patients affected by IF/SBS and CD patients at high risk of developing IF, to identify disease severity-related biomarkers.
Methods:
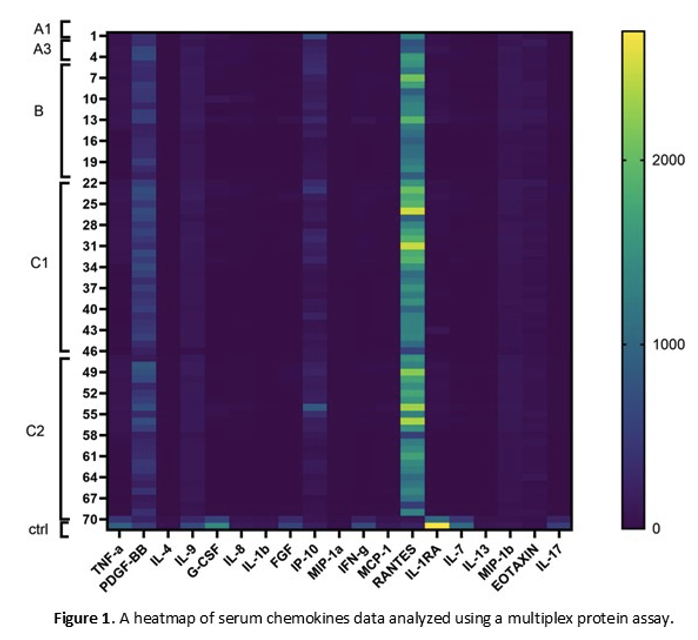
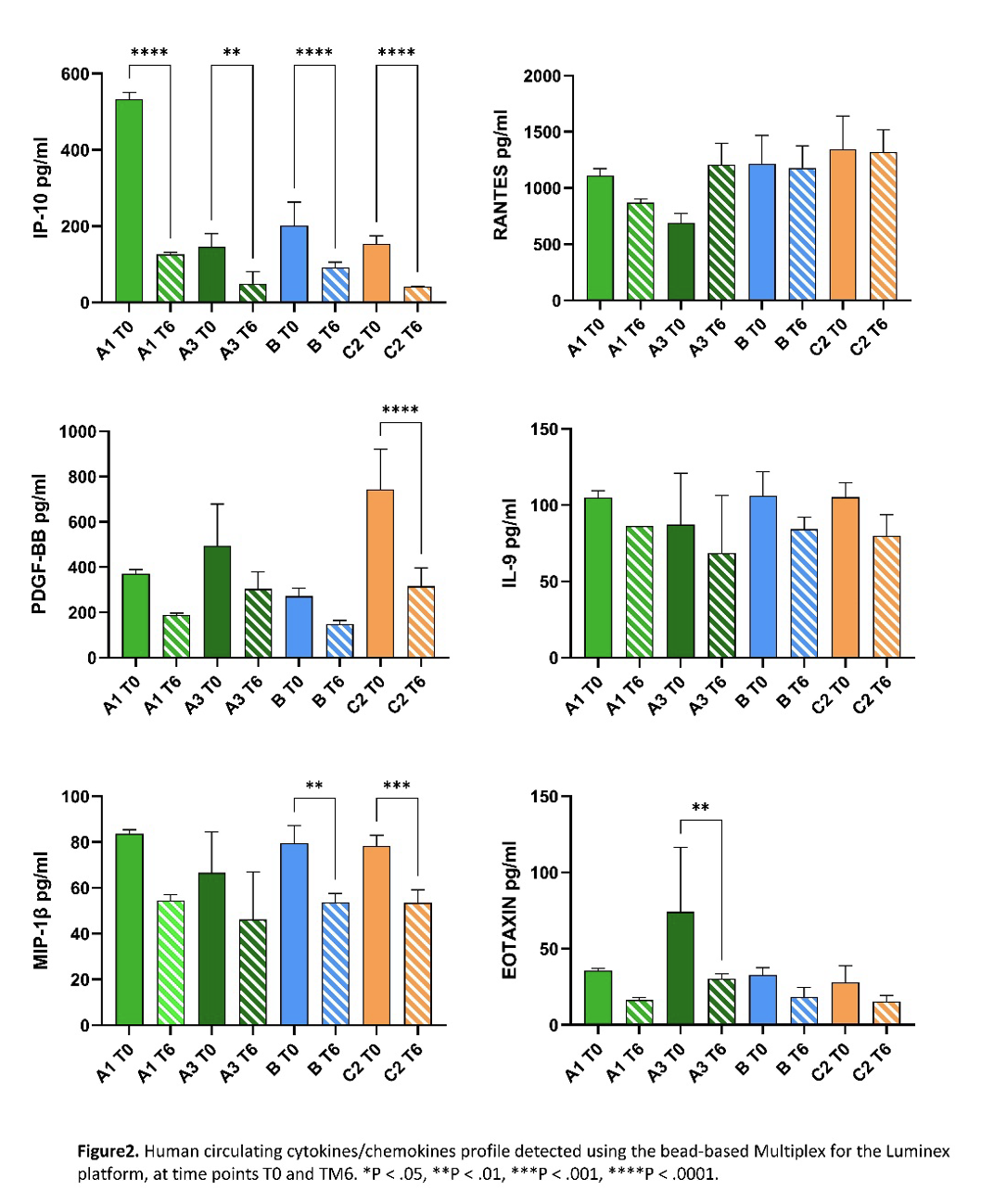
A total of 150 CD patients were enrolled in this study, and they were stratified into four subgroups based on the disease severity: SBS patients with IF and parenteral nutrition (A1 group) or without IF and inactive disease (A3 group); CD patients with high (B group) or low risk of IF (C2 group). Circulating cytokine and chemokine levels were determined using the human 27-PLEX assay on sera collected from patients at the time of enrollment (T0, n = 70) and after 6 months (T6, n = 10).
Results:
Comparisons between groups highlighted divergent cytokine signatures correlating with disease severity and nutritional support requirements. Serum cytokines and chemokines profiling at baseline (T0) and after six months (T6) revealed distinct inflammatory patterns across the study groups. Patients with SBS and IF (group A1) showed persistently elevated levels of IP-10, IL-12, MIP-1α, and G-CSF, reflecting sustained immune activation. Whereas patients at high risk of IF (group B) displayed increased levels of Eotaxin, bFGF, IL-15, and IL-6, indicative of subclinical inflammation and possible tissue remodeling. A general reduction in cytokine levels was observed at T6 compared to T0, although anti-inflammatory mediators remained minimally modulated, suggesting ongoing low-grade inflammation.
Conclusions:
The differences in the levels of cytokines/chemokines among the various patient groups suggest that specific circulating cytokines may serve as potential biomarkers for the early identification of patients at risk of IF. Literature data also confirmed a role for these cytokines/chemokines in CD severity and progression3,4. However, further large-scale studies are needed to validate these preliminary results and to fully establish their prognostic significance.
Bibliography:
- Friedrich M, Pohin M, Powrie F. Cytokine Networks in the Pathophysiology of Inflammatory Bowel Disease. Immunity. 2019;50(4):992-1006. doi:10.1016/j.immuni.2019.03.017
- Singh UP, Singh NP, Murphy EA, et al. Chemokine and cytokine levels in inflammatory bowel disease patients. Cytokine. 2016;77:44-49. doi:10.1016/j.cyto.2015.10.008
- Mello JDC, Gomes LEM, Silva JF, et al. The role of chemokines and adipokines as biomarkers of Crohn’s disease activity: a systematic review of the literature. Am J Transl Res. 2021;13(8):8561-8574.
- Ansari N, Abdulla J, Zayyani N, Brahmi U, Taha S, Satir AA. Comparison of RANTES expression in Crohn’s disease and ulcerative colitis: an aid in the differential diagnosis? J Clin Pathol. 2006;59(10):1066-1072. doi:10.1136/jcp.2005.034983
VALUTA ABSTRACT
Vota ogni categoria
| Originality | |
| Clarity | |
| Rationale | |
| Objectives | |
| Endpoint measures | |
| Statistics | |
| Results | |
| Relevance | |
|
Media
|
|

|
|