AREA TEMATICA: General gastro
Authors:
Luigi Colecchia, MD*,1,2, Giovanni Marasco, MD, PhD*,1,2, Cecilia Capelli, MD1,2, Antonio Facciorusso, MD3, Marcello Fabio Maida, MD4, Alessandro Vitello, MD4, Elton Dajti, MD1,2, Maria Raffaella Barbaro, PhD1,2, Arianna Gobbato, MD1,2, Cesare Cremon, MD1,2, Giovanni Barbara, MD1,2.
Affiliations:
- Department of Medical and Surgical Sciences, University of Bologna, Bologna, Italy
- IRCCS Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy
- Department of Experimental Medicine, Università del Salento, 73100 Lecce, Italy
- Department of Medicine and Surgery, University of Enna Kore, Enna, Italy
Background and aims:
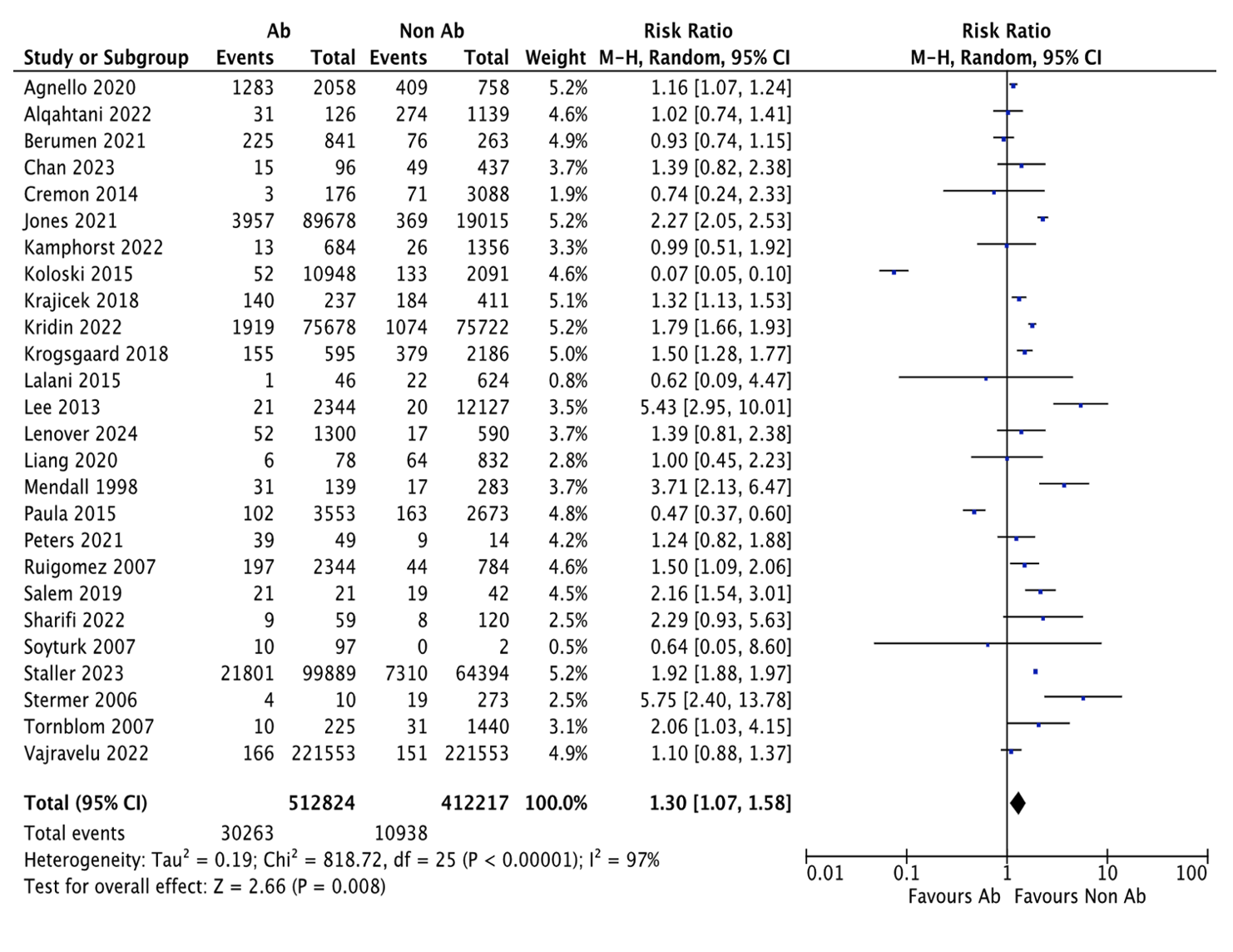
Irritable bowel syndrome (IBS) is a disorder of gut-brain interaction which negatively affects patients’ quality of life. It has been hypothesized that changes in gut microbiota composition and function evoked by antibiotic use represent a trigger for IBS development. This systematic review and meta-analysis aims to assess the incidence of IBS following antibiotic use.
Methods:
Medline, Embase, and Scopus, along with relevant conference abstracts and citation tracking were searched up to June 15th, 2025. Studies that reported new diagnoses of IBS in patients with documented antibiotic exposure versus controls without antibiotic exposure were included. Data extraction and quality assessment were performed independently by two reviewers. Pooled incidence rates per 1000 person-years, along with incidence rate ratios (IRRs) with 95% confidence intervals (CI) were pooled; heterogeneity was expressed as I2. Meta-regression analysis was performed to assess the impact of confounding covariates.
Results:
Thirty-one studies comprising a total of 422,350 patients (244,632 antibiotic users and 177,718 non-users) were included. The overall pooled incidence of IBS was 26% in antibiotic users compared to 20% in non-users, resulting in an IRR of 1.3 (95% CI: 1.07–1.58; p = 0.008). In sensitivity analyses including only studies in which antibiotics were used for gastrointestinal infections, the risk of developing IBS was higher for antibiotic users (IRR: 1.71; 95% CI: 1.16–2.51; p = 0.007), with high heterogeneity (I² > 90%) among studies. Meta-regression analysis showed that the geographical area where the study was carried out and criteria used for IBS diagnosis were associated with high heterogeneity.
Conclusions:
Antibiotic use is associated with increased risk of developing IBS, especially following gastrointestinal infections. However, the significant study heterogeneity reduces the power of our results, suggesting that further high-quality research is needed to clarify this relationship.
VALUTA ABSTRACT
Vota ogni categoria
| Originality | |
| Clarity | |
| Rationale | |
| Objectives | |
| Endpoint measures | |
| Statistics | |
| Results | |
| Relevance | |
|
Media
|
|

|
|