AREA TEMATICA: General gastro
Authors:
Luigi Colecchia1, Francesco Candia2, Arianna Gobbato3, Anna Rita Di Biase2, Sara Crestani2, Giulia Cammarata2, Valentina Boarino4, Elton Dajti1, Federico Ravaioli1, Cesare Cremon1, Antonio Colecchia4, Lorenzo Iughetti2, Giovanni Barbara1, Giovanni Marasco1
Affiliations:
- Department of Medical and Surgical Sciences (DIMEC), University of Bologna, Bologna, Italy
- Department of Medical and Surgical Science of Mother, Children and Adult – Pediatric Unit, University of Modena & Reggio Emilia, University Hospital of Modena and Reggio Emilia, Modena, Italy
- Department of Medical and Surgical Sciences – Pediatric Unit, University of Bologna, Bologna, Italy
- Gastroenterology Unit, Department of Medical Specialities (CHIMOMO), University of Modena and Reggio Emilia, Modena, Italy
Background and aims:
Patients with celiac disease (CD) can present persistence or de-novo occurrence of gastrointestinal symptoms later in life even following a strict gluten-free diet (GFD). Indeed, GFD can alter the gut microbiota inducing dysbiosis that with time may lead to the development of disorders of gut-brain interaction (DGBI). In this prospective study, we evaluated the rate of irritable bowel syndrome (IBS), functional dyspepsia (FD), anxiety, and depression over a follow-up period of more than 10 years in a population of patients with CD following GFD.
Methods:
Patients with CD diagnosed between 2004 to 2014 were re-evaluated after an average 12,5 years on GFD to assess the presence of DGBI. Rome-IV (pediatric modules if patients were younger than 17 years old), gastrointestinal symptoms rating scale (GSRS) and hospital anxiety and depression scale (HADS) questionnaires were administered along with the evaluation of the last blood examinations. The rates of IBS, FD, anxiety, and depression were then assessed. Univariate and multivariate analyses were performed to investigate the presence of factors associated with IBS and FD.
Results:
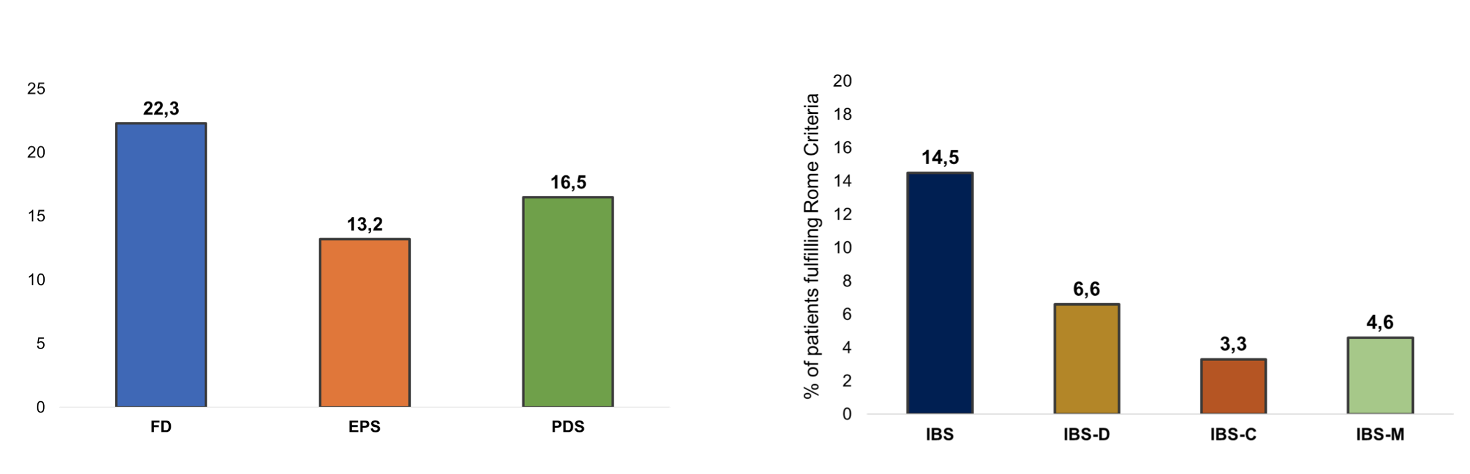
We contacted 197 patients. Patients who were not strictly adhering to GFD (25 patients) and who did not complete the questionnaires (20 patients) were excluded from the study. We finally included 152 patients (77%). The median follow-up time was 154 months (125-180). The rate of IBS was 14.47% (22/152) which increased to 22.3% (21/94) considering only the adult population. Patients were then subclassified in IBS-C (5/22, 22.7%), IBS-M (6/22, 27.3%), and IBS-D (10/22, 45.5%). The overall rate of FD was 7.24% (11/152): 11.7% (11/94) in the adult population and none in the pediatric one. We found that postprandial distress syndrome (PDS) was present in 7.89% (12/152) of the population and epigastric pain syndrome (EPS) in 5.26% (8/152). Significantly higher rates of anxiety were found in patients developing IBS and FD (Table 1 and 2). Univariate and multivariate analyses showed that a longer follow-up time was significantly correlated to a higher rate of IBS and that anxiety was correlated with both IBS and FD.
Conclusions:
Over more than 10 years from the initial diagnosis of CD, we found a higher rate of IBS and FD than the one reported for the general population. In our cohort, IBS and FD diagnoses are correlated with higher levels of anxiety and longer follow-up time.
Table 1. Patients characteristics and uni- and multivariate analyses assessing risk factors for IBS development in celiac disease patients in gluten-free diet
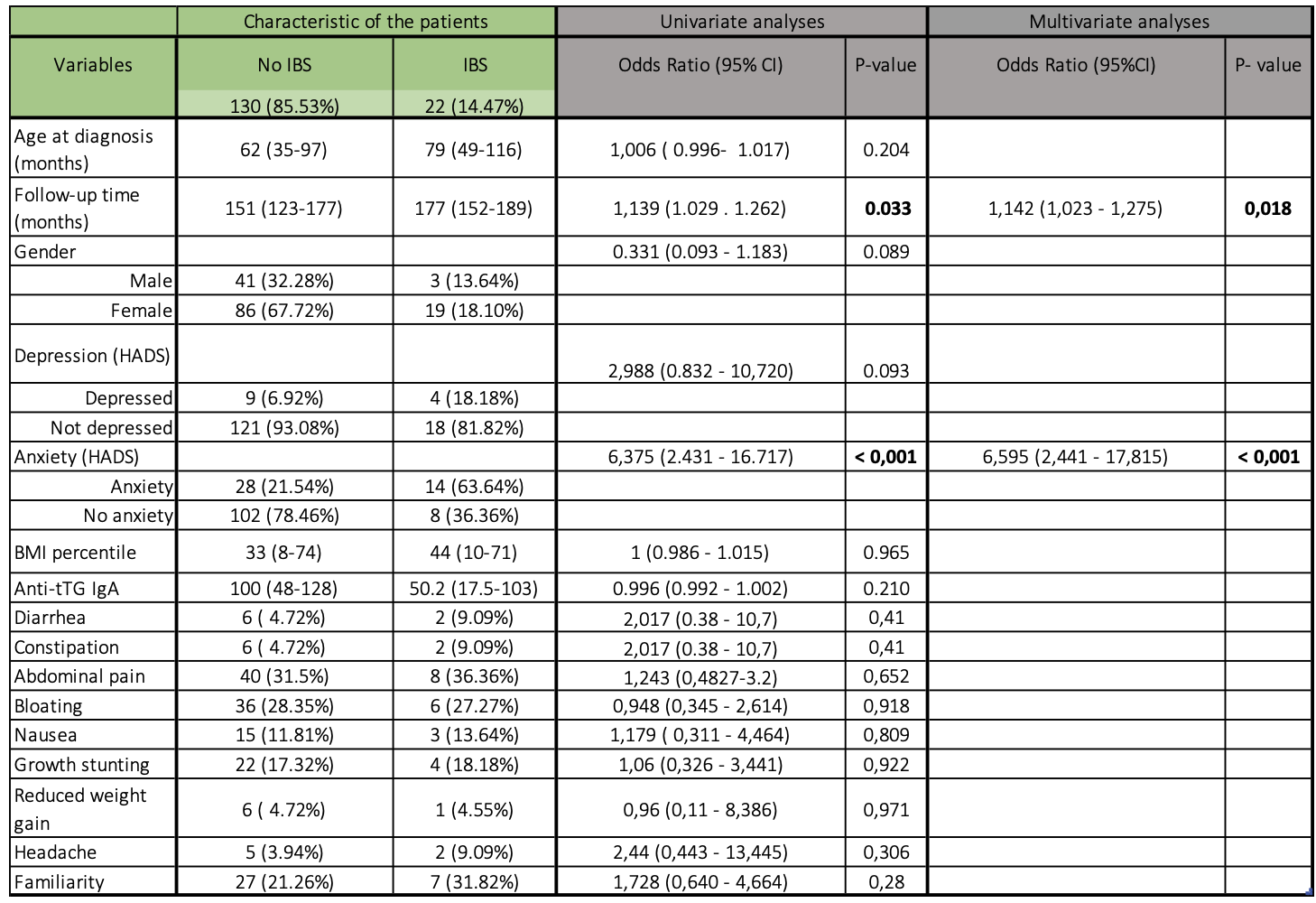
Table 2. Overall FD and IBS rates in the population in 152 CD patients assessed after a median follow-up of 12.5 years.
VALUTA ABSTRACT
Vota ogni categoria
| Originality | |
| Clarity | |
| Rationale | |
| Objectives | |
| Endpoint measures | |
| Statistics | |
| Results | |
| Relevance | |
|
Media
|
|

|
|