AREA TEMATICA: Endoscopia
Authors:
Roberta De Maron, Stefano Siboni, Carlo Galdino Riva, Jiurgen Mema, Marco Sozzi, Emanuele Asti
Affiliations:
Unità Operativa di Chirurgia Generale e d’Urgenza, IRCCS Policlinico San Donato, Milano, Università degli studi di Milano
Background and aims:
Gastroesophageal reflux disease (GERD) is a common and complex disorder, primarily driven by anti-reflux barrier (ARB) disruption. According to Lyon 2.0, upper-GI endoscopy (EGD) provides definitive diagnostic criteria (1), and allows a direct view of the esophago-gastric junction (EGJ). The traditional Hill classification lacks precision and clinical significance due to its exclusive focus on the muscolo-mucosal flap valve (FV) without standardized measures of hiatal hernia (HH) or hiatal opening. The American Foregut Society (AFS) classification, introduced in 2022, evaluates and integrates three EGJ components, axial length of HH (L), diameter of hiatal opening (D), and FV (F), allowing to phenotype of the EGJ (2). This study aims to assess whether the AFS classification better stratifies GERD severity compared to Hill and to weight the single AFS component contribution to the overall pathophysiology of GERD
Methods:
A retrospective analysis of a prospective database of adult patients (18-75 years) evaluated for GERD symptoms at our Institution (December 2022-May 2025) was performed. Inclusion criteria were EGD, high-resolution manometry (HRM), and reflux monitoring. Exclusion criteria were prior foregut surgery or major esophageal disorders. GERD was defined by Lyon 2.0 criteria. EGJ was assessed during EGD using AFS (L, D, F components) and Hill classifications. GERD prevalence, DeMeester score, mean nocturnal baseline impedance (MNBI), and Milan Score were explored within the AFS phenotypes and compared across AFS and Hill grades and number of disrupted AFS components. Logistic regression assessed AFS component contributions, and receiver operating characteristic (ROC) analysis compared classification performance.
Results:
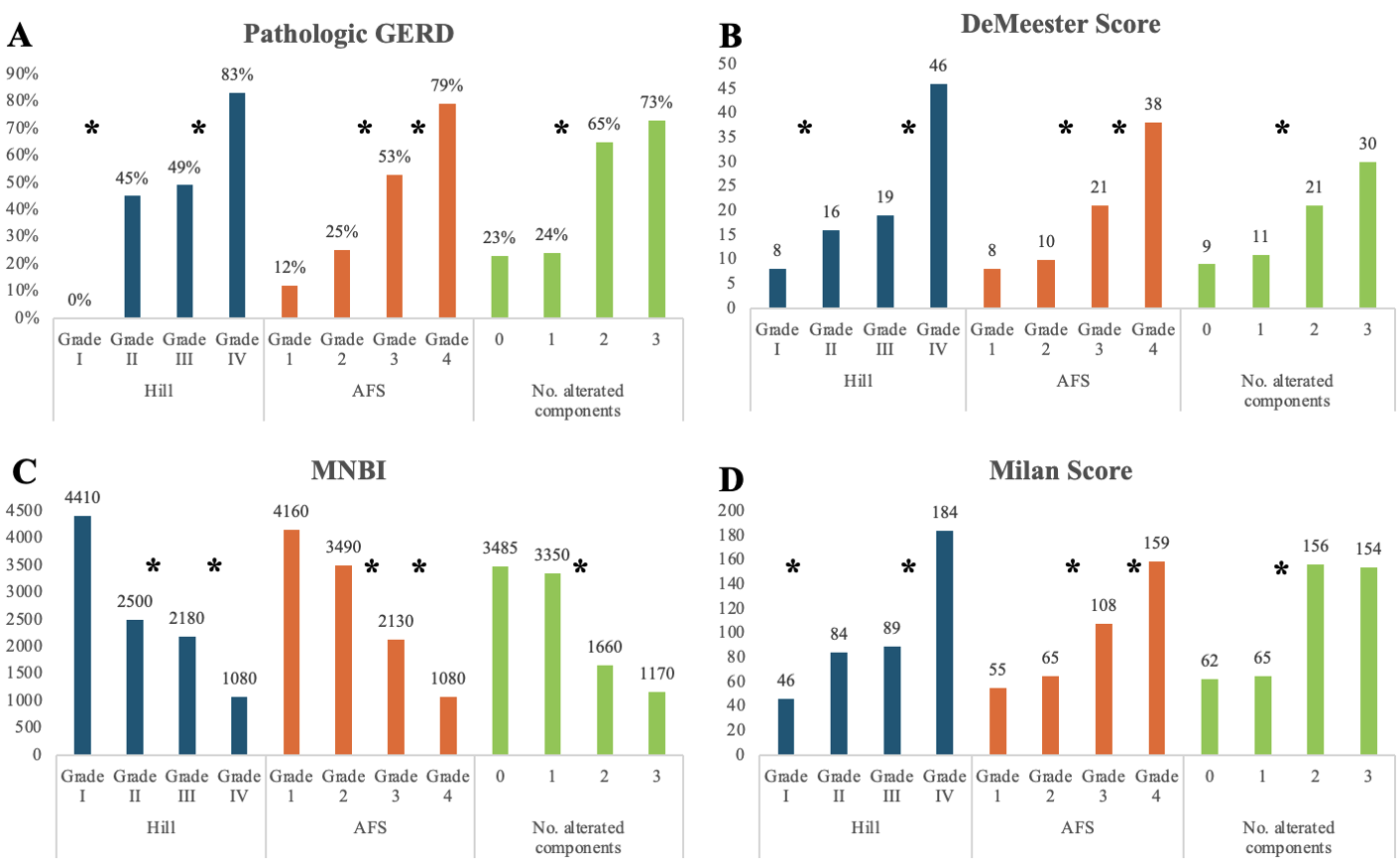
Of 249 patients (median age 52, 47% male, BMI 23.9 kg/m²), 127 had GERD. GERD patients were older, predominantly male, with higher BMI. At least one AFS component was disrupted in 71.9% of the patients (59.2% all three, 22.3% two, 18.4% one). We observed a stepwise increase of GERD rate across the AFS phenotypes (Table 1). GERD prevalence, DeMeester score, MNBI, and Milan Score differed significantly across AFS grades 1-2 vs. 3 and 3 vs. 4, unlike Hill grades, where 2 and 3 overlapped. Considering the number of components disrupted, patients with 1 and 2 impaired components were significantly different from those with 3 and 4 (Figure 1). Logistic regression found pathologic D (OR 2.537) and F (OR 3.336) as independent GERD predictors, but not L (p=0.543). ROC analysis confirmed AFS superiority (AUC 0.750 vs. Hill 0.653, p<0.001).
Conclusions:
In conclusion, our study demonstrates that the AFS classification enhances the diagnostic yield of EGD, providing an accurate quantification of the ARB disruption.
Bibliography:
- Gyawali CP, Yadlapati R, Fass R, et al. Updates to the modern diagnosis of GERD: Lyon consensus 2.0. Gut. 2024 Jan 5;73(2):361-371. doi: 10.1136/gutjnl-2023-330616. PMID: 37734911; PMCID: PMC10846564.
- Nguyen NT, Thosani NC, Canto MI, et al. The American foregut society white paper on the endoscopic classification of esophagogastric junction integrity. Foregut. 2022;2(4):339-348. doi:10.1177/26345161221126961
Table 1. Distribution of AFS phenotypes and prevalence of GERD in each phenotype.
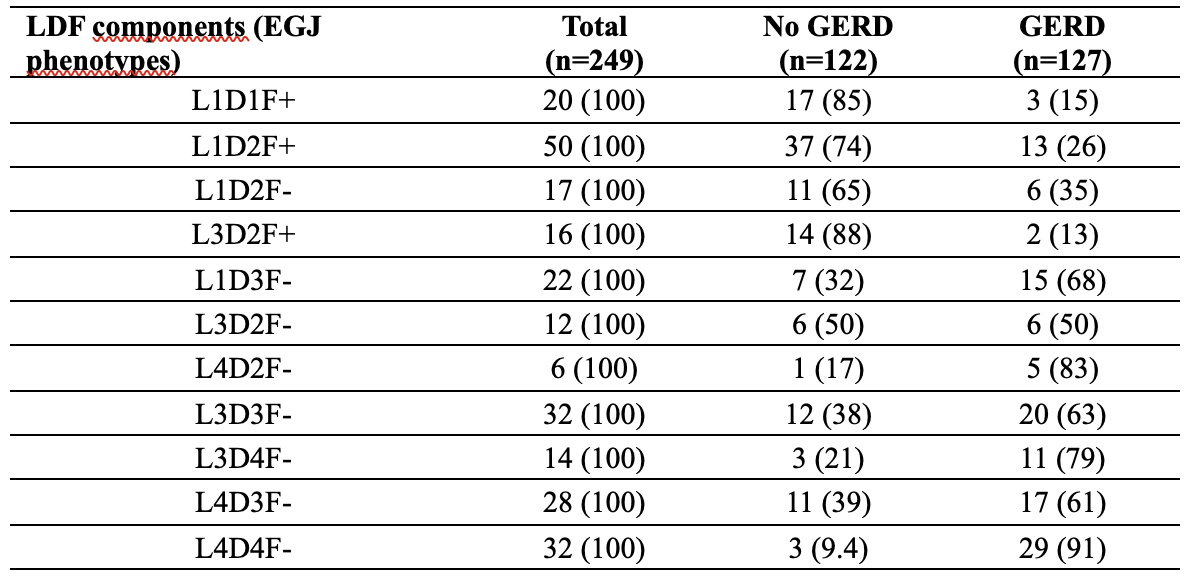
Figure 1. Trend and comparison of A) incidence of pathologic GERD, B) values of DeMeester Score, C) values of MNBI and D) values of Milan Score between Hill and AFS classification and among their grades. AFS: American Foregut Society; GERD: Gastro-Esophageal Reflux Disease; MNBI: Mean Nocturnal Baseline Impedance.
VALUTA ABSTRACT
Vota ogni categoria
| Originality | |
| Clarity | |
| Rationale | |
| Objectives | |
| Endpoint measures | |
| Statistics | |
| Results | |
| Relevance | |
|
Media
|
|

|
|