AREA TEMATICA: Endoscopia
Authors:
Stefano Fantasia1, Stefano Kayali1,2, Pablo Cortegoso Valdivia2,3, Stefano Andreotti1, Daniele Macchi1, Giorgio Nervi2, Nico Pagano4, Luigi Laghi1,2,5
Affiliations:
- Department of Medicine and Surgery, University of Parma, Parma, Italy
- Gastroenterology and Endoscopy Unit, University Hospital of Parma, Parma, Italy
- Faculty of Health Sciences, University of Southern Denmark, Odense, Denmark
- Gastroenterology Unit, Department of Oncological and Specialty Medicine, University Maggiore Hospital della Carità, Novara
- Laboratory of Molecular Gastroenterology, Humanitas Clinical and Research Centre, Rozzano, Milan, Italy
Background and aims:
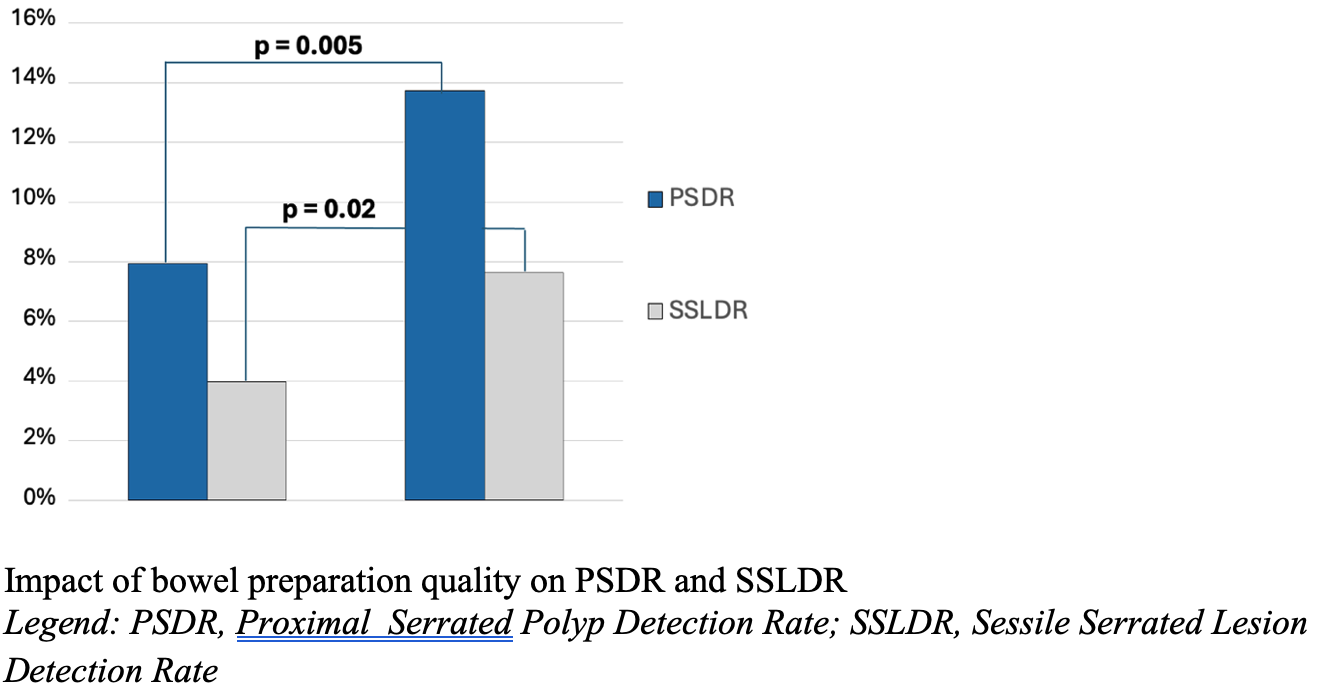
The Proximal Serrated Polyp Detection Rate (PSDR) is an emerging quality indicator linked to post-colonoscopy colorectal cancer risk, but the benefit of bowel cleanliness on its detection remains unclear. We evaluate the impact of excellent (Boston Bowel Preparation Scale [BBPS] 8–9) versus good (BBPS 6–7) preparation on serrated (PSDR and sessile serrated lesion detection rate [SSLDR]) and adenoma-related (adenoma detection rate [ADR] and adenoma per colonoscopy [APC]) quality indicators in a FIT-positive screening cohort.
Methods:
This retrospective single-center study of 1069 patients (age 50–69) undergoing screening colonoscopy after a positive FIT compared PSDR, SSLDR, ADR, and APC between excellent and good preparation groups using univariate and multivariate regression analyses.
Results:
Excellent preparation showed a significantly higher PSDR (13.7% vs. 7.9%; OR 1.84, 95%CI 1.22–2.80, p=0.004) and SSLDR (7.6% vs. 4.0%; OR 2.00, 95%CI 1.14-3.52, p=0.016) than good cleansing. A linear relationship was observed, BBPS 9 outperforming BBPS 8. No significant difference was found for ADR (50.4% vs. 47.9%; OR 1.10, 95%CI 0.87-1.41, p=0.424) and APC (MD=0.103; 95% CI, -0.071-0.277, p=0.247).
Conclusions:
Aiming for an excellent rather than a good bowel preparation is a critical strategy to maximize the detection rate of serrated pathway lesions and potentially reduce the incidence and mortality for interval colorectal cancer (CRC). This benefit does not extend to adenoma detection, underscoring the importance of PSDR and SSLDR as distinct and complementary quality indicators.
Bibliography:
- Rex DK, et al. Am J Gastroenterol. 2012;107:1315–1329.
- Zhao S, et al. Gastroenterology. 2019;156:1661–1674.
- Nishihara R, et al. N Engl J Med. 2013;369:1095–1105.
Figure 1.
VALUTA ABSTRACT
Vota ogni categoria
| Originality | |
| Clarity | |
| Rationale | |
| Objectives | |
| Endpoint measures | |
| Statistics | |
| Results | |
| Relevance | |
|
Media
|
|

|
|